Join The MRIoA Team
MRIoA is a growing company that provides an exceptional, positive work environment. We are committed to our employees and consistently seek talented, highly motivated individuals to join our team.
Employees of MRIoA can expect a career that is both challenging and rewarding. Your individual performance contributes to our success and each employee is appreciated and valued for the skills, ideas and experience they bring to their position.
We offer a generous compensation package, including competitive wages and comprehensive benefits. MRIoA is an equal opportunity employer.

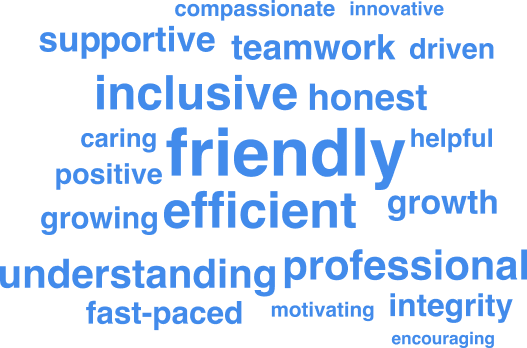
How Our Employees Describe Our Culture
Organizational Strengths Of Medical Review Institute Of America
Execution
Employees think things run efficiently and well
Clued-In Employees
Employees feel Informed about important decisions
Meetings
Employees feel meetings make good use of their time
Our Employees Say MRIoA Operates By Strong Values
93% of employees think that MRIoA operates by Strong Values
Employee Testimonials
Join The Medical Reviewer Panel
Our reviewers are located nationwide and are clinical experts in their areas of specialization while they remain in active clinical practice. When cases are referred by MRIoA, they review Prior Authorizations or Appeals for treatment to see if they meet nationally accepted medical and health plan guidelines. Reviewers provide their expertise as an unbiased, external source, and in compliance with ERISA/DOL and/or state laws.












